In my youth I worked for a paid ambulance service, and while we all lived for the emergency calls, the routine transports were the calls that paid the bills. Compared with the glamor and excitement of a lights-and-siren run to a car wreck or heart attack, transports were dull as dirt. And dullest of all were the daily runs from nursing homes to the dialysis center, where rows of comfy chairs sat, each before a refrigerator-sized machine designed to filter the blood of a patient in renal failure, giving them another few days of life.
Sadly, most of those patients were doomed; many were in need of a kidney transplant for which there was no suitable donor, while some were simply not candidates for transplantation. Dialysis was literally all that stood between them and a slow, painful death, and I could see that at least some of them were cheered by the sight of the waiting dialysis machine. The principles of how the kidneys work have been known since at least the 1800s, but it would take until 1945 for the efforts of a Dutch doctor, using used car parts and sausage casings, to make the predecessor of those machines: the first artificial kidney.
Restoring Balance
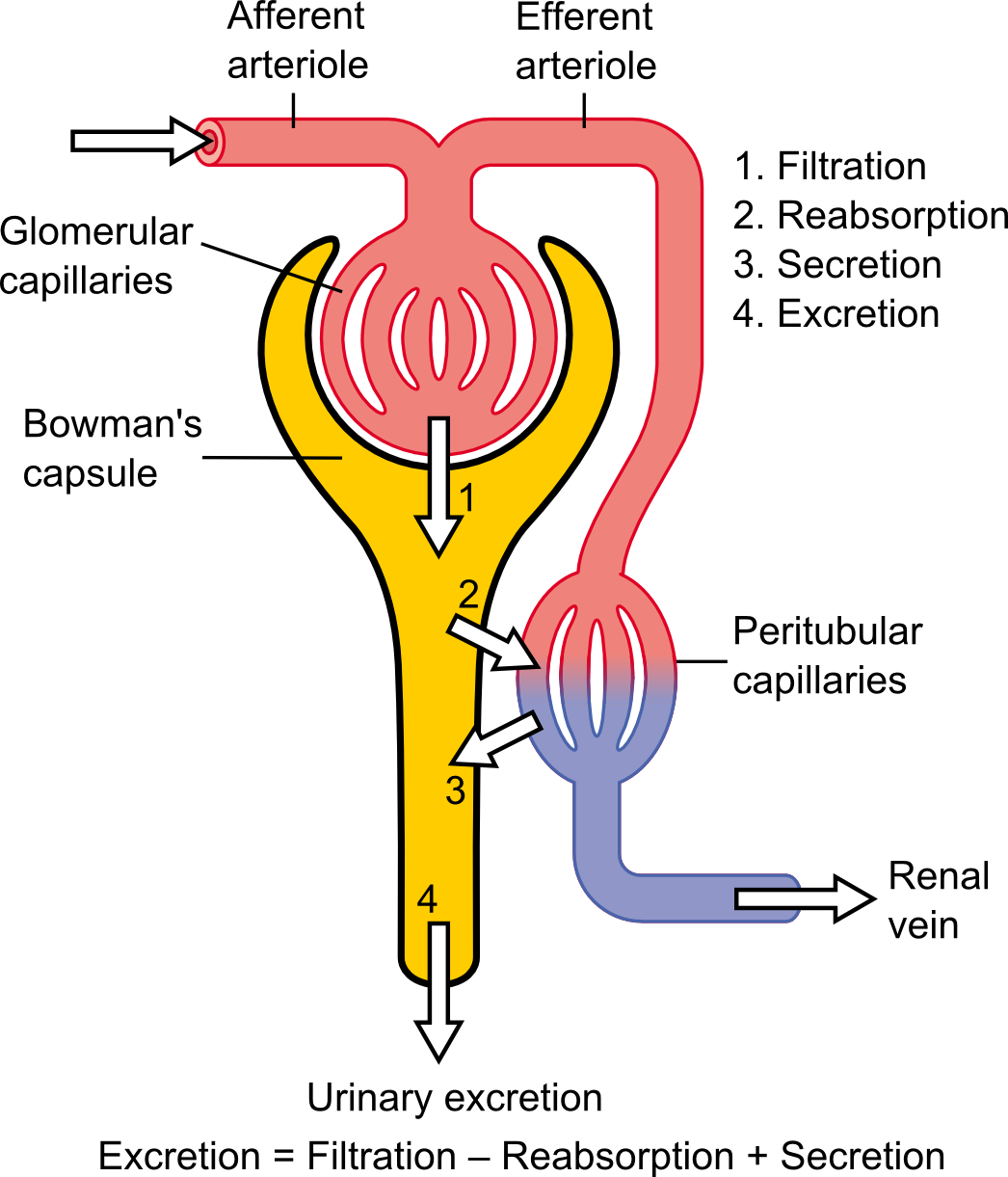
We’ve all likely seen the principle behind this demonstrated at some point in school. Osmosis is the tendency of solutions to seek a balance between solvent and solute across semipermeable membranes such as biological tissues. In the kidney, blood plasma (the solvent) containing nitrogenous waste (the solute) flows through capillaries (the semipermeable membrane). The other side of the membrane is a structure called the Bowman’s capsule, into which flows the nitrogenous waste along with a fair amount of sodium chloride, glucose, and amino acids. Most of the water and some of the solutes in that filtrate are reabsorbed by capillaries further along the Bowman’s capsule, with the balance excreted as urine.
Healthy kidneys are a marvel of efficiency, filtering the entire volume of plasma in the body 60 times a day. Of the 180 liters of the bulk filtrate produced almost all of it is reabsorbed, leaving behind about 2 liters of urine to be eliminated. Without the kidneys, the body would be unable to maintain fluid balance, blood pH, and the correct concentrations of vital electrolytes. Nausea, vomiting, and edema would follow quickly; the inevitable death would be slow and gruesome, as a young Dr. Willem Kolff would learn first hand.
No Way to Die

In 1938, a 22-year-old man entered the hospital at the University of Groningen in the Netherlands in acute renal failure. Dr. Kolff, fresh out of medical school and barely older than his patient, was put in charge of the case. There really wasn’t much to do; while Dr. Kolff knew exactly what was happening – up to 20 grams of urea were accumulating in the man’s body every day, slowly poisoning him – there was no way to remove it. Dr. Kolff could do little but watch helplessly as the man died.
Keen to find a way to save such patients, Dr. Kolff began looking for ways to “jump start” the kidneys. For several years he looked for drugs to stimulate the kidneys to improve their function, but found none. Then history took an unexpected turn and the world went to war. When the Germans swept through the Netherlands, Dr. Kolff happened to be in The Hague. As Nazi bombers swarmed overhead, he went to the hospital and volunteered to set up a blood bank. After four days of scrounging equipment and supplies and dodging Nazi snipers, the hospital’s first blood bank was in operation. It remains in operation to this day.
To avoid the worst of the Nazi occupation, he left the university hospital and headed for Kampen, a smaller city. The hospital there was glad for the help and paid the young internist enough to start working on his kidney treatments again. This time, he would concentrate on an artificial kidney.
Dr. Kolff had done experiments with cellophane sausage casings. He filled them with blood that had been spiked with urea and placed them in a saline solution. After some time and agitation, the urea had moved across the semipermeable cellophane membrane into the salt bath, removing it from the blood inside. He had the basis for an artificial kidney.
Cellophane and Salt Water
His expertise with blood banks would now come in handy. Handling blood in large volumes outside the body is not a trivial task, and doing so gave Dr. Kolff the confidence that a machine to do the job of a kidney was possible. He knew from his experiments that he’d need 10 meters of sausage casing, and that both the blood and the saline solution would need to be circulated. He built a drum from wooden slats and suspended it on an axle so that half its diameter was in a laundry tub. The cellophane tubing was wrapped around the drum and the tub was filled with saline. The tubing was filled with the patient’s blood, and a motor gently rotated the drum through the saline bath. When the blood had been cleaned, it would be returned to the patient.

The artificial kidney was crude, and initially not terribly effective. Of the first 15 patients treated with it in Kampen, only one survived, and Dr. Kolff admits she might have lived without the treatment. It would not be until 1945 that dialysis would have its first unequivocal success: a 67-year-old woman in prison for collaborating with the Nazis. Dr. Kolff was urged to let her die, but he dialyzed her and she came out of her coma. She survived for seven more years. The artificial kidney had proven itself.
Closer to the Heart
Having conquered dialysis and shared his designs freely with doctors all over the world, in 1950 Dr. Kolff was offered a job at the prestigious Cleveland Clinic. There his interests turned to other artificial organs, including the problems of open-heart surgery. At the time there was no way to bypass the heart during surgery, so he set about building one of the first membrane oxygenators, a machine that pumps blood over a porous plastic membrane to oxygenate the blood while removing carbon dioxide. This eventually let coronary artery bypass surgery become a common surgical procedure, with 200,000 performed in the United States alone every year.
Dr. Kolff also turned his inventive mind to the artificial heart. In fact, the first implantable artificial heart, the Jarvik-7, was one of Kolff’s designs. It was named after Dr. Robert Jarvik, one of Kolff’s students and the project manager on the team. In 1981 the Jarvik-7 was implanted in Barney Clark, who survived 112 days before succumbing to multiple systems failure.
Dr. Willem Kolff had a long and storied career, eventually retiring at age 86. His artificial organs, especially his artificial kidney, have saved countless lives, and continue to be used to this day. That they started with something as mundane as sausage casing and a laundry tub full of salt water only makes the achievement more impressive.
No comments:
Post a Comment